Despite advancements in surgery, radiotherapy, and chemotherapy, the prognosis for
patients with malignant gliomas and cerebral metastases remains poor, with a mean survival for
patients with high-grade gliomas of only 12-15 months. One major reason for poor survival is
that it remains difficult to distinguish tumor from non-tumor tissue on standard imaging,
providing limited information for guiding biopsies or performing complete neurosurgical resection of malignant tissue. Since the extent of surgical removal of high-grade tumors correlates with overall survival and quality of life, as well as response to radiation and
chemotherapy, advanced imaging techniques that provide better delineation of tumors are of critical importance to patient care.
In recent years, a special type of imaging, diffusion weighted imaging (DWI), has gained
increased popularity within neuro-oncology for identifying regions of a malignant tumor on magnetic resonance images. DWI is a technique that measures the movement of water molecules within the brain, and it has shown some promise for identifying areas of hindered diffusion associated with highly cellular tumors. However, there are several pitfalls of DWI including its sensitivity to edema and necrosis. Indeed, mouse models and clinical studies of patients with high-grade gliomas have demonstrated that imaging parameters obtained from DWI are often unreliable in differentiating tumor from surrounding edema.
In order to address this problem, the researchers and clinicians at the Center for Translational Imaging and Precision Medicine (CTIPM) have recently developed an innovative, advanced imaging technique called Restriction Spectrum Imaging (RSI) that overcomes many of the known limitations of DWI. Unlike standard DWI, RSI is able to isolate areas of “restricted diffusion” (i.e., areas where tumor cells restrict the movement of water) without being influenced by edema and other non-tumor tissue within and surrounding the tumor.
The Neuro-Imaging team at CTIPM, which includes Dr. Nikdokht Farid, Dr. Anders Dale, Dr. Nathan White, and Dr. Carrie McDonald, have shown that by isolating areas of restricted diffusion, RSI can significantly (1) improve the conspicuity of high-grade primary and metastatic brain tumors on MRI, (2) improve the ability to visualize white matter tracts coursing through regions of peritumoral edema and (3) facilitate the interpretation of tumor response on imaging following treatment with anti-angiogenic agents (e.g. bevacizumab).
Images from a 50-year-old man with glioblastoma multiforme (GBM)
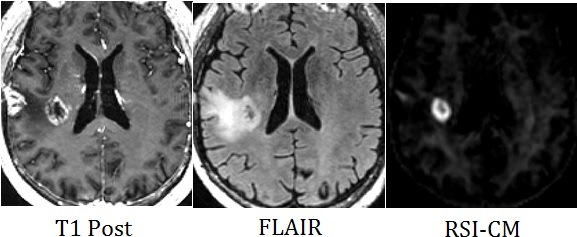
He had previously undergone biopsy of his right temporal lobe GBM, and had subsequently received radiation therapy. These images following radiation show an area of contrast enhancement and edema in the right temporal lobe. Based on standard imaging, these findings could either represent persistent tumor or changes related to radiation therapy. However, the RSI cellularity map (RSI-CM) clearly shows a ring-like area of high RSI signal in this region, indicating an area of high cellularity due to persistent tumor. Therefore, due to the conspicuity of the area of persistent tumor on RSI-CM, the neuro-surgeon and neuro-oncologist were able to determine the correct management for this patient, who was sent to surgery for resection of the residual tumor.
Images from another patient with a high-grade glioma in the left occipital lobe
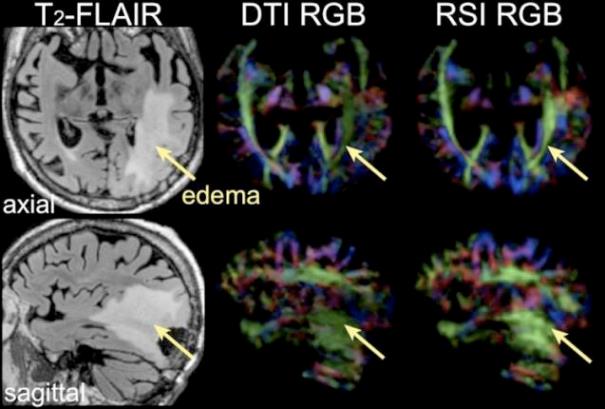
There is quite a bit of edema surrounding the tumor in the posterior left temporal and occipital lobes, as seen on the T2-FLAIR image. The fractional anisotropy (FA) RGB maps next to the FLAIR image show the white matter tracts coursing adjacent to the tumor (i.e. the inferior longitudinal fasciculus (ILF)). Although the RGB map derived from standard diffusion tensor imaging (DTI) shows the ILF, it appears thin and attenuated. This is due to the extensive peritumoral edema. In contrast, the RGB map derived from RSI demonstrates a robust ILF, despite the peritumoral edema. This is because RSI and RSI-derived parameters are not influenced by edema. The ability to visualize a robust ILF adjacent to the tumor was critically important for this patient’s care, because it allowed the neurosurgeon to determine that this important white matter tract was intact and that special attention should be given to avoid injuring this tract during surgery.
These examples demonstrate that RSI has great potential for improving the management of patients with primary and metastatic brain tumors. At CTIPM, we will leverage RSI’s strengths to assist our neurosurgery, neuro-oncology, and radiation oncology colleagues to provide more accurate diagnoses, to better assess response to treatment, and to improve outcomes following surgery and radiation.