Active Research
Regulation of Vacular and Neuro Inflammation via Targeted Cholesterol Efflux: Role of AIBP
Oxidized Lipids and Vascular Inflammation
Previous Areas of Interest
Zebrafish Models of Lipid Abnormalities and Vascular Disorders

Aortic root aherosclerotic leasions (credit: Colin Agatisa-Boyle)

Spinal cord (credit: Juliana Navia Pelaez)
Program Overview
The unifying theme in the research program in Miller’s laboratory is the role of cholesterol and lipid metabolism and lipid oxidation in fundamental biologic processes and in the development of human disease. The discoveries of the oxidized lipoprotein function in activating toll-like receptors (TLRs) and of the role of apoA-I binding protein (AIBP) in regulation of lipid raft dynamics, made in our lab, has connected lipid metabolism with inflammation. We pioneered the use of zebrafish in studying vascular lipid accumulation and inflammation, and continue to create new transgenic zebrafish lines with lipid abnormalities and with genetic reporters to detect oxidized lipids. This work led to our recent discoveries of novel functions of lipid metabolism in regulation of vascular and neuro inflammation, neuropathic pain and angiogenesis.
Oxidized Lipids and Vascular Inflammation
Vascular lipid accumulation and vascular inflammation are major pathogenic processes in the development of atherosclerosis. Inflammation promotes lesion growth and its development into a vulnerable plaque. But why is vascular lipid accumulation per se leading to inflammatory responses by vascular cells? The hypothesis my colleagues and I have developed proposes that lipoprotein oxidation, which inevitably occurs in lipid-rich vascular lesions, creates agonists for innate immune receptors (1).
Our discovery that oxidized cholesterol esters (OxCE) induce inflammatory responses in macrophages via TLR4/MD2 (2-5) supports this hypothesis. The finding that an OxCE activates TLR4, the receptor for bacterial LPS, was further supported by the recognition of structural homology between plasma LPS-binding protein (LBP) and cholesterol ester transfer protein (CETP), and between MD2, which binds LPS, and NPC2, a lysosomal cholesterol ester binding protein. Importantly, we have shown the presence of specific OxCE moieties, which activate TLR4/MD2, in human plasma and in human coronary plaques (5,6).
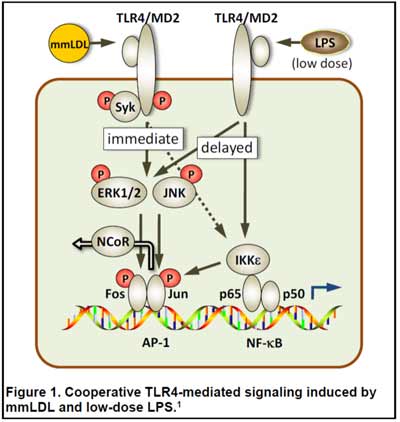 Emerging evidence suggests that persistent subclinical endotoxemia is an integral component of metabolic disorders induced by Western type, high-fat diets, and has been termed "metabolic endotoxemia." We have demonstrated that injections of low doses of LPS and minimally oxidized LDL (mmLDL) cooperatively (and even synergistically) activate macrophages in a TLR4-dependent manner to express higher levels of proinflammatory cytokines (Fig. 1) (1,7). We are currently testing the hypothesis that metabolic endotoxemia, induced by a high-fat diet, together with OxCE, a component of atherosclerotic lesions, synergistically enhance vascular inflammation.
Emerging evidence suggests that persistent subclinical endotoxemia is an integral component of metabolic disorders induced by Western type, high-fat diets, and has been termed "metabolic endotoxemia." We have demonstrated that injections of low doses of LPS and minimally oxidized LDL (mmLDL) cooperatively (and even synergistically) activate macrophages in a TLR4-dependent manner to express higher levels of proinflammatory cytokines (Fig. 1) (1,7). We are currently testing the hypothesis that metabolic endotoxemia, induced by a high-fat diet, together with OxCE, a component of atherosclerotic lesions, synergistically enhance vascular inflammation.
Zebrafish Models of Lipid Abnormalities and Vascular Disorders
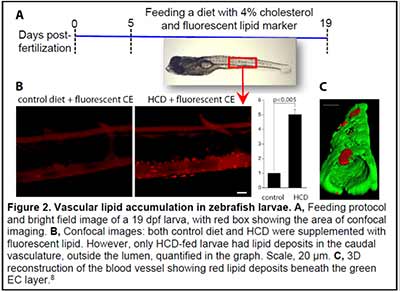
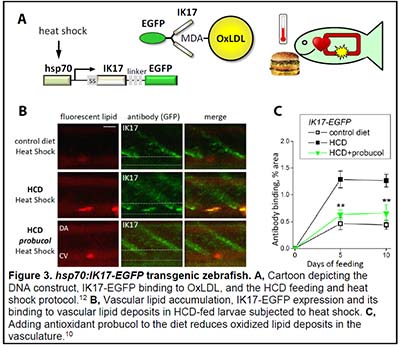
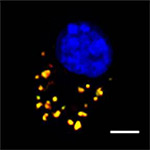
We have become fascinated by the zebrafish animal model because of the optical transparency of zebrafish larvae and the possibility to observe developmental, physiologic and pathologic processes in live animals. We have developed imaging and analytic techniques to study in vivo vascular lipid accumulation and leukocyte recruitment, endothelial disorganization and vascular permeability, and lipoprotein oxidation (Figs. 2 and 3) (8-13). In collaboration with Drs. Witztum and Tsimikas, we developed a transgenic zebrafish with conditional expression of the malondialdehyde (MDA)-specific human antibody IK17 conjugated with EGFP (Fig. 3) (10). The IK17-EGFP transgene was placed under control of the hsp70 promoter. A heat shock of such a hsp70:IK17-EGFP zebrafish induced transient secretion of IK17-EGFP and enabled us to image MDA epitopes at specific time points of vascular lesion development and test protective roles of antioxidants and regression diets (10).
We are also developing genetic models of lipid disorders. Our apoc2 knockout zebrafish display a strong hypertriglyceridemia phenotype and pancreas growth abnormalities (14). New transgenic lines overexpressing zebrafish pcsk9 and apoa1 and human ALOX15, as well as the line deficient in lpl are currently being propagated and analyzed.
Regulation of Angiogenesis and Inflammation via Targeted Cholesterol Efflux: Role of AIBP
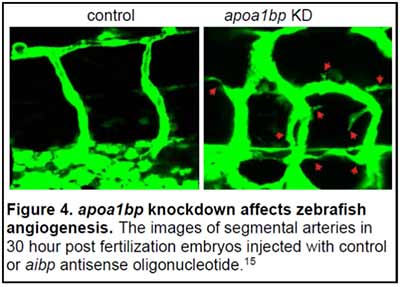
ApoA-I Binding Protein (AIBP, human gene APOA1BP) is a secreted, 29 kDa protein, which is ubiquitously expressed in many cell types and tissues. We discovered that extracellular AIBP accelerated cholesterol efflux from endothelial cells (EC) to HDL, the process mediated by the cellular cholesterol transporter ABCG1 (15). AIBP/HDL-mediated cholesterol efflux disrupted lipid rafts in the EC plasma membrane, which in turn interfered with VEGFR2 signaling and inhibited angiogenesis. We found that in embryonic zebrafish, the AIBP-mediated cholesterol efflux was essential for proper angiogenesis. The knockdown of AIBP in zebrafish resulted in dysregulated angiogenesis, characterized by excessive branching and sprouting of growing blood vessels (Fig. 4). In a gain-of-function experiment, ectopic expression of AIBP inhibited segmental artery sprouting from the dorsal aorta (15).
This new mechanistic link between cholesterol metabolism and angiogenesis opens numerous avenues to study the role of cholesterol efflux in general and of AIBP in particular in angiogenesis during development, in post-ischemic heart, when revascularization of the myocardium is beneficial to the patient, and in cancer, where inhibition of tumor vascularization is an important therapeutic strategy. We also plan to study the role of AIBP in lipid metabolism and in the development of atherosclerosis and other chronic inflammatory diseases. We are captivated by the prospect of AIBP as a therapy. Administration of recombinant AIBP may prevent hyper-inflammatory response in acute conditions as well as restrict chronic inflammatory responses. Elucidating mechanisms of anti-inflammatory responses to AIBP treatment and exploring its beneficial effects in various animal models of acute and chronic inflammatory diseases is a major focus of our studies.
References
- Miller YI, Choi S-H, Wiesner P, Fang L, Harkewicz R, Hartvigsen K, Boullier A, Gonen A, Diehl CJ, Que X, Montano E, Shaw PX, Tsimikas S, Binder CJ, Witztum JL. Oxidation-specific epitopes are danger associated molecular patterns recognized by pattern recognition receptors of innate immunity. Circ Res. 2011;108:235-248.
- Miller YI, Viriyakosol S, Binder CJ, Feramisco JR, Kirkland TN, Witztum JL. Minimally modified LDL binds to CD14, induces macrophage spreading via TLR4/MD-2, and inhibits phagocytosis of apoptotic cells. J Biol Chem. 2003;278:1561-1568.
- Miller YI, Viriyakosol S, Worrall DS, Boullier A, Butler S, Witztum JL. Toll-like receptor 4-dependent and -independent cytokine secretion induced by minimally oxidized low-density lipoprotein in macrophages. Arterioscler Thromb Vasc Biol. 2005;25:1213-1219.
- Choi S-H, Harkewicz R, Lee JH, Boullier A, Almazan F, Li AC, Witztum JL, Bae YS, Miller YI. Lipoprotein accumulation in macrophages via toll-like receptor-4-dependent fluid phase uptake. Circ Res. 2009;104:1355-1363.
- Choi S-H, Yin H, Ravandi A, Armando A, Dumlao D, Kim J, Almazan F, Taylor AM, McNamara CA, Tsimikas S, Dennis EA, Witztum JL, Miller YI. Polyoxygenated cholesterol ester hydroperoxide activates TLR4 and SYK dependent signaling in macrophages. PLoS One. 2013;8:e83145.
- Ravandi A, Leibundgut G, Hung MY, Patel M, Hutchins PM, Murphy RC, Prasad A, Mahmud E, Miller YI, Dennis EA, Witztum JL, Tsimikas S. Release and capture of bioactive oxidized phospholipids and oxidized cholesteryl esters during percutaneous coronary and peripheral arterial interventions in humans. J Am Coll Cardiol. 2014;63:1961-1971.
- Wiesner P, Choi SH, Almazan F, Benner C, Huang W, Diehl CJ, Gonen A, Butler S, Witztum JL, Glass CK, Miller YI. Low doses of lipopolysaccharide and minimally oxidized low-density lipoprotein cooperatively activate macrophages via nuclear factor {kappa}B and activator protein-1. Possible mechanism for acceleration of atherosclerosis by subclinical endotoxemia. Circ Res. 2010;107:56-65.
- Stoletov K, Fang L, Choi SH, Hartvigsen K, Hansen LF, Hall C, Pattison J, Juliano J, Miller ER, Almazan F, Crosier P, Witztum JL, Klemke RL, Miller YI. Vascular lipid accumulation, lipoprotein oxidation, and macrophage lipid uptake in hypercholesterolemic zebrafish. Circ Res. 2009;104:952-960.
- Fang L, Harkewicz R, Hartvigsen K, Wiesner P, Choi SH, Almazan F, Pattison J, Deer E, Sayaphupha T, Dennis EA, Witztum JL, Tsimikas S, Miller YI. Oxidized cholesteryl esters and phospholipids in zebrafish larvae fed a high-cholesterol diet: macrophage binding and activation. J Biol Chem. 2010;285:32343-32351.
- Fang L, Green SR, Baek JS, Lee SH, Ellett F, Deer E, Lieschke GJ, Witztum JL, Tsimikas S, Miller YI. In vivo visualization and attenuation of oxidized lipid accumulation in hypercholesterolemic zebrafish. J Clin Invest. 2011;121:4861-4869
- Baek JS, Fang L, Li AC, Miller YI. Ezetimibe and simvastatin reduce cholesterol levels in zebrafish larvae fed a high-cholesterol diet. Cholesterol. 2012;2012:564705.
- Fang L, Miller YI. Emerging applications for zebrafish as a model organism to study oxidative mechanisms and their roles in inflammation and vascular accumulation of oxidized lipids. Free Radic Biol Med. 2012;53:1411-1420.
- Fang L, Liu C, Miller YI. Zebrafish models of dyslipidemia: relevance to atherosclerosis and angiogenesis. Transl Res. 2013.
- Liu C, Gates KP, Fang L, Amar MJ, Schneider DA, Geng H, Huang W, Kim J, Pattison J, Zhang J, Witztum JL, Remaley AT, Dong PD, Miller YI. Apoc2 loss-of-function zebrafish mutant as a genetic model of hyperlipidemia. Dis Model Mech. 2015;8:989-998.
- Fang L, Choi SH, Baek JS, Liu C, Almazan F, Ulrich F, Wiesner P, Taleb A, Deer E, Pattison J, Torres-Vazquez J, Li AC, Miller YI. Control of angiogenesis by AIBP-mediated cholesterol efflux. Nature. 2013;498:118-122.
Information to come.
NEWS from the Miller Laboratory
August 2018 - new R21 REVERSAL OF PREEXISTING NEUROPATHIC PAIN BY SPINAL DELIVERY OF AIBP, with Tony Yaksh (UCSD)

May 2018 - Dina Schneider defended her PhD Thesis
Congrats, Dina!
August 2017 - new R01 AIBP AND REGULATION OF NEUROPATHIC PAIN, with Tony Yaksh (UCSD)
August 2017 - new Project CHOLESTEROL REGULATION OF INFLAMMATORY MACROPHAGES IN ATHEROSCLEROSIS in the Program Project Grant IMMUNE CELL INTERACTIONS IN ATHEROSCLEROSIS, collaborative program with Chaterine (Lynn) Hedrick, Klaus Ley (both La Jolla Immunology Institute) and Coleen McNamara (University of Virginia)
February 2017 - Yury Miller has been awarded an Outstanding Investigator Award (R35) AIBP THERAPY from the NHLBI

January 2016
Chao Liu has been awarded an American Heart Association postdoctoral fellowship. Congratulations! |
 | August 2015 Chao Liu published a new paper in Disease Models & Mechanisms. The image from his work is on the cover of the August issue and the paper is highlighted "In This Issue." Apoc2 loss-of-function zebrafish mutant as a genetic model of hyperlipidemia. Liu C, Gates KP, Fang L, Amar MJ, Schneider DA, Geng H, Huang W, Kim J, Pattison J, Zhang J, Witztum JL, Remaley AT, Dong PD, Miller YI. Dis Model Mech. 2015 Aug 1;8(8):989-98. doi: 10.1242/dmm.019836. |
| | |
 | May 2015 Soo-Ho Choi published a new paper in Autophagy. SYK regulates macrophage MHC-II expression via activation of autophagy in response to oxidized LDL. Choi SH, Gonen A, Diehl CJ, Kim J, Almazan F, Witztum JL, Miller YI. Autophagy. 2015;11(5):785-95. doi: 10.1080/15548627.2015.1037061. |